Scroll to:
Modification of the anastomotic technique in completely laparoscopic resection rectopexy with NOSE — a case report
https://doi.org/10.24060/2076-3093-2022-12-1-56-60
Abstract
Introduction. We have come a long way from the era of conventional rectal surgery, with most high-volume centres now practising various degrees of laparoscopy assisted colorectal surgeries, via extracorporeal suturing, ex vivo anastomoses, hand-assisted laparoscopic resection anastomoses to robotic rectal resections. However, the limitation to most such techniques remains the fact that these are not ‘completely’ laparoscopic, with varying degrees of open assistance being required, from mobilization, suturing and anastomoses to specimen extraction via separate abdominal incisions or port-site enlargements. These ‘large’ incisions negate some of the advantages of minimal access surgery and lead to complications at such sites, such as wound breakdown, infections, and incisional herniae. This led to the origin of NOTES (Natural Orifice Translumenal Endoscopic Surgery) and the still fairly new concept of NOSE (Natural Orifice Specimen Extraction).
Aim. We aim to describe our application of this new frontier in laparoscopic colorectal surgery, doing away with large scars prone to complications.
Materials and methods. We describe a case of completely laparoscopic resection rectopexy and trans-rectal extraction of the specimen, with a modified technique of anvil insertion, enabling the faster creation of a larger anastomosis with probably lower anastomotic morbidity.
Results and discussion. The patient underwent a ‘completely’ laparoscopic resection rectopexy and had an uneventful immediate post-operative recovery. She had no delayed post-operative complications or recurrence of the rectal prolapse and remained free of constipation as well, over a follow-up period of 6 months.
Conclusion. We conclude that this modification of the surgical technique reduces operative time, allows use of larger circular staplers, theoretically reducing the incidence of anastomotic stricture, and being easily reproducible, can be widely applied for better cosmetic and functional outcome.
Keywords
For citations:
Mohanty A. Modification of the anastomotic technique in completely laparoscopic resection rectopexy with NOSE — a case report. Creative surgery and oncology. 2022;12(1):56-60. https://doi.org/10.24060/2076-3093-2022-12-1-56-60
Introduction
Rectal prolapse is an uncommon, though distressing condition, often affecting elderly multiparous women. Other risk factors include musculoskeletal, connective disorders, psychiatric illness and obesity [1–3]. The prolapse maybe limited to mucosa, but often it is full-thickness, and extruded portion is exposed to trauma, bleeding, perforation and trophic ulceration, with some patients presenting with spurious diarrhoea while others maybe constipated [3]. The surgical approach has broadly been transabdominal versus perineal, with the latter being preferred in the reproductive age group in the early days of laparoscopic approach to the pelvis. However, with the advent of more refined techniques, laparoscopic rectosigmoid resections with transabdominal specimen extraction have come into vogue [4][5].
However, the additional scars on the abdomen used for the hand-port or specimen extraction caused pain and dissatisfaction in some patients, defeating the purpose of a totally laparoscopic approach and adding a risk of herniation at these sites. In recent years, some researchers have reported trans-anal specimen extraction [6–8] in malignant and benign rectal pathology. Transrectal-NOSE is a good option for specimen extraction and the creation of an intra-corporeal colorectal anastomosis because of its applicability in both sexes and its frequent indications in left-sided colonic disease [9].
Rectal fixation utilizing synthetic materials is being increasingly avoided due to associated complications such as infection of prosthetic mesh, bowel erosion and obstruction [10][11]. Hence, at our centre, resection rectopexy is completed by intracorporeal suturing of the rectosigmoid to the presacral fascia using non-absorbable suture material. There are different techniques described to achieve the colorectal anastomosis, including trans-anal exteriorization of colon and laparoscopic purse string application We describe here a case report of totally laparoscopic resection of the prolapsed rectosigmoid, with trans-rectal NOSE, and an intra-corporeal stapled anastomosis with a novel technique for the introduction of the anvil into the descending colon stump, doing away with the need for exteriorization of the colon and the subsequent need for further mobilization or the need for a purse-string at the colonic stump after anvil insertion.
Materials and methods
Case report
A 67-year-old lady presented to our outpatient with symptoms of a mass descending per annum for 6 months, with gradual increase in size. She had a BMI of 29.5, had been constipated for several years, had a history of laxative abuse, and was a postmenopausal multipara with 4 vaginal deliveries. She had a history of intermittent loose stools for a month. An examination revealed a scaphoid unremarkable abdomen with previous surgical scars, and a 15 cm long rectal procidentia. There was no trophic ulcer and the prolapse was reducible with some degree of effort and discomfort. She was evaluated and after due consenting, was taken up for a laparoscopic resection rectopexy.
Surgical technique
The patient was prepared in a low lithotomy position with arms at the side, with 4 ports placed (yellow star — 12 mm port, blue star — 5 mm port). The surgeon and first assistant stood at the right of the patient with the second assistant shifting between the left and between the legs (Fig. 1).
The dissection was carried out as in conventional laparoscopic resection of the rectosigmoid, with the patient in a steep Trendelenberg, left side up position, for the most part. The uterine fundus was hitched with a transabdominal prolene stitch, to keep it out of the stapler’s path. After circumferential mobilization of the rectum upto the levator ani, the redundancy was marked by clips and the segment was divided proximally and distally, using the bipolar scissors, ensuring that there was no significant contamination. The resected specimen was extracted trans-rectally using a sponge holder, while the rectal stump was stabilized with laparoscopic Babcock forceps (Fig. 2). The anvil of a 33 mm circular EEA was then introduced via the rectal stump (Fig. 3), detached from the handle by a heavy angled forceps and directed into the lumen of the proximal colonic stump. The anvil tip was positioned against the tinea libera of the colon and an incision was created at this point, 4 cm proximal to the stump (Fig. 4). The anvil tip was extruded on the antimesenteric border of the proximal colon, without purse-string application. The open ends of the proximal descending colon and the distal rectum were closed with a green cartridge (4.5 mm) of endo-GIA 60 mm linear stapler (Fig. 5).
The mobilized colon was brought close to the rectal stump and the EEA stapler handle was gently introduced toward the staple line, the tip being extruded under vision at the staple line (Fig. 6). The anvil and handle were re-attached securely and the EEA knob rotated till optimally fixed (Fig. 7). The anastomosis was completed and the stapler was withdrawn trans-anally. An underwater leak test was performed by blowing air using a rigid sigmoidoscope, while at the same time visually inspecting the staple line for defects or bleeding. The rectum was fixed by 2-0 prolene sutures to the presacral fascia, at 3 points on either side, 1 cm apart, using a simple interrupting technique (Fig. 8). A 28 Fr. tube drain was left in the pelvis, being extruded via the left flank 5 mm port site. 12 mm port site sheaths were closed using a standard fascia closure stitch, and the procedure was thus completed.
The patient was allowed oral fluids on POD 1, followed by soft diet the next day. She was discharged in a stable condition, after drain removal, on the 4th POD. Clip removal was performed on the 8th POD, at which time she had no evidence of recurrence. She was followed closely for 6 months post-surgery, by which time, she had no recurrence, and her constipation had resolved as well.
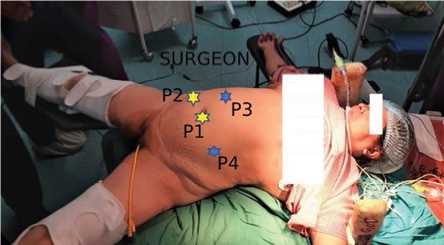
Figure 1. Port and patient positioning
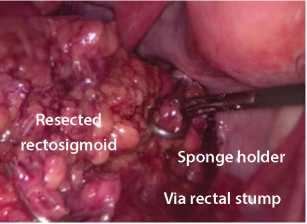
Figure 2. Transrectal specimen extraction
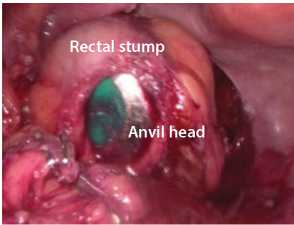
Figure 3. CEEA introduced via rectal stump
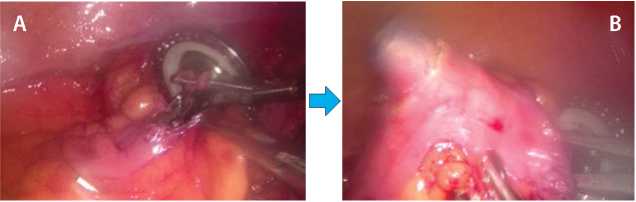
Figure 4. A — anvil introduced into proximal colon; B — anvil tip extruded along tinea libera

Figure 5. Endo GIA 4.5, 60mm green cartridge closure of colonic opening

Figure 6. CEEA needle via rectal staple line
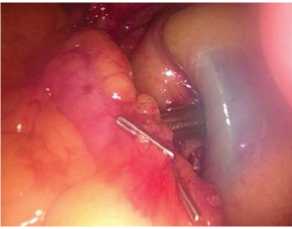
Figure 7. Mating of anvil tip and needle

Figure 8. Sutured rectopexy being performed
Results and discussion
Many theories have been put forward regarding the aetiology of rectal prolapse. However, the uniform relationship between rectoanal intussusception and ‘dolichosigmoid’ with constipation in prolapse patients has been confirmed using defaecography and cineradiographic studies [8][12]. Resection of redundant rectosigmoid becomes mandatory when there is a history of constipation with or without an obvious dolichosigmoid [13]. Resection along with synthetic or isograft sling rectopexy were the standard of care at the outset; however, over the past three decades, the trend has shifted in favour of resection with sutured rectopexy alone [14]. There is abundant data in favour of laparoscopy-assisted performance of these procedures, but the natural orifice specimen extraction technique, leading to more technically demanding anastomotic challenges, has been sparingly reported. An article [8] reported a totally intracorporeal handsewn anastomotic technique compared to an intracorporeal anvil placement similar to ours, but with the anvil pushed head-first into the colonic stump, and the tip secured by purse string suture placement.
We find that such a technique is feasible with the smaller 31 mm CEEA staple anvil, but with the larger, 33 mm CEEA, placing the head directly within the descending colon stump is both time-consuming and causes significant trauma to the bowel mucosa, theoretically increasing the risk of an anastomotic leak. The technique described in this paper does away with the need to apply a purse-string altogether and at the same time, it is technically easier to pull the anvil trocar out through a tinea libera incision on the colonic wall, where the larger anvil head enters the bowel in a diametric fashion, leading to less stretching and injury, in contrast to the other technique, where it has to enter by stretching the bowel to the circumference of the anvil head, an ordeal in a small calibre colon. The 2 mm larger anastomosis achieved with the 33 mm CEEA should lead to better functional outcomes and a lower incidence of anastomotic strictures, though this remains to be established by further controlled and powered studies.
Conclusion
Natural orifice specimen extraction has added a new frontier to the ever-evolving progress in truly minimal access surgery, and along with NOTES, may achieve actual scarless surgery in more dramatic procedures as well. We believe that our modification of the anvil placement technique will not only save time and avoid additional suturing, but also achieve a better functional outcome, with less morbidity to the proximal colonic mucosa, preventing anastomotic leaks in the immediate post-operative period and stricture in the long run, enabling anastomosis with larger stapler sizes.
Written informed consent was obtained from the patient for publication of this case report and accompanying materials.
The authors declare no conflict of interest.
This work is not funded.
References
1. Joubert K., Laryea J.A. Abdominal approaches to rectal prolapse. Clin Colon Rectal Surg. 2017;30(01):57–62. DOI: 10.1055/s-0036-1593426
2. Felt-Bersma R.J., Bartelsman J.F. Haemorrhoids, rectal prolapse, anal fissure, peri-anal fistulae and sexually transmitted diseases. Best Pract Res Clin Gastroenterol. 2009;23(4):575–92. DOI: 10.1016/j.bpg.2009.04.010
3. Bordeianou L., Hicks C.W., Kaiser A.M., Alavi K., Sudan R., Wise P.E. Rectal prolapse: an overview of clinical features, diagnosis, and patient-specific management strategies. J Gastrointest Surg. 2014;18(5):1059–69. DOI: 10.1007/s11605-013-2427-7
4. Zhou T, Zhang G, Tian H, Liu Z, Xia S. Laparoscopic rectal resection versus open rectal resection with minilaparotomy for invasive rectal cancer. J Gastrointest Oncol. 2014 Feb;5(1):36–45. DOI: 10.3978/j.issn.2078-6891.2013.052
5. Koulas S.G., Pappas-Gogos G., Spirou S., Roustanis E., Tsimogiannis K.E., Tsirves G., et al. Evaluations of laparoscopic proctocolectomy versus traditional technique in patients with rectal cancer. JSLS. 2009;13(4):564–73. DOI: 10.4293/108680809X12589998404489
6. Franklin M.E. Jr, Liang S., Russek K. Integration of transanal specimen extraction into laparoscopic anterior resection with total mesorectal excision for rectal cancer: a consecutive series of 179 patients. Surg Endosc.2013;27(1):127–32. DOI: 10.1007/s00464-012-2440-z
7. Kim S.J., Choi B.J., Lee S.C. A novel single-port laparoscopic operation for colorectal with transanal specimen extraction: a comparative study. BMC Surg. 2015;15(1):10. DOI: 10.1186/1471-2482-15-10
8. Rajkumar J.S., Prabhakaran R., Akbar S., Rajkumar A.J., Venkatesan G., Rajkumar S. Totally laparoscopic resection rectopexy with transanal extraction of the specimen. Saudi Surg J. 2018;6:89–93. DOI: 10.4103/ssj.ssj_5_18
9. Guan X., Liu Z., Longo A., Cai J.C., Tzu-Liang Chen W., Chen L.C., et al. International consensus on natural orifice specimen extraction surgery (NOSES) for colorectal cancer. Gastroenterol Rep (Oxf). 2019;7(1):24–31. DOI: 10.1093/gastro/goy055
10. Lundby L., Iversen L.H., Buntzen S., Wara P., Høyer K., Laurberg S. Bowel function after laparoscopic posterior sutured rectopexy versus ventral mesh rectopexy for rectal prolapse: a double-blind, randomised single-centre study. Lancet Gastroenterol Hepatol. 2016;1(4):291–7. DOI: 10.1016/S2468-1253(16)30085-1
11. Marghich O., Benichou B., Amouzou E.-G., Maubert A., Etienne J. H., Benizri E., et al. Case series of mesh migration after rectopexy surgery for rectal prolapse. J Surg Case Rep. 2022;2022(2):rjac017. DOI: 10.1093/jscr/rjac017
12. Rao S.S., Rattanakovit K., Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat Rev Gastroenterol Hepatol. 2016;13(5):295–305. DOI: 10.1038/nrgastro.2016.53
13. Poljo A., Klugsberger B., Klimbacher G., Schimetta W., Shamiyeh A. Clinical outcome after resection rectopexy in patients with constipation and rectal prolapse. Ann Colorectal Res. 2021;9(1):2–7. DOI: 10.30476/acrr.2021.90321.1089
14. Sahoo M.R., Thimmegowda A.K., Gowda M.S. A single centre comparative study of laparoscopic mesh rectopexy versus suture rectopexy. J Minim Access Surg. 2014;10(1):18–22. DOI: 10.4103/0972-9941.124456
About the Author
A. MohantyIndia
Senior Consultant, Department of General, Minimal Access and G.I. Surgery,
Delhi
Review
For citations:
Mohanty A. Modification of the anastomotic technique in completely laparoscopic resection rectopexy with NOSE — a case report. Creative surgery and oncology. 2022;12(1):56-60. https://doi.org/10.24060/2076-3093-2022-12-1-56-60
JATS XML


































