Scroll to:
The Complication Of Decrease In Aorto-Mesenteric Angle And Distance Its Diagnosis And Treatment: Case Report
https://doi.org/10.24060/2076-3093-2022-12-2-123-127
Abstract
Introduction. Wilkie syndrome is a pathological manifestation caused by an abnormal disorder of the superior mesenteric artery arising from the abdominal part of the aorta. As a result, the distal part of the duodenum is compressed between the abdominal aorta, spine, and SMA, which creates a hindrance for the passage of himus in the duodenum, creating a mechanical obstruction.
Aim: To draw the surgeons’ attention towards the possibility of developing a rare complication of decreased aorto-mesenteric angle and the distance, highlighting the challenges in diagnosis and treatment.
Materials and methods. This article presents a clinical case of WS diagnosed in the surgical department of the BSMU clinic. We hereby discuss the case report of a 28-year-old patient diagnosed at the initial stage of WS. The patient had been suffering from the symptoms of WS since 2018 but wasn’t able to identify the disease, but when he came to the surgical department of BSMU clinic based on the results of abdominal CT-scan with combined contrast of the stomach and duodenum per os with water-soluble contrast and computer angiography of the mesenteric vessels, the diagnosis was confirmed. The patient was treated with the duodenojejunostomy (laparoscopic Strong’s operation).
Results and discussion. Absence of timely diagnosis of this disease can lead to life-threatening complications, and early diagnostics is complicated by similarity of initial manifestations with other gastropancreaticoduodenal diseases. One of the most promising approach in the diagnosis of Wilkie syndrome is the use of abdominal CT-scan with combined contrasting of the stomach and duodenum per os with water-soluble contrast and computer angiography of vessels. In the present clinical case due to the given combination of methods we can assess functional state of the stomach and duodenum, clearly visualize not only the organs topography but also estimate the aorto-mesenteric angle and distance, which can further determine the type and tactics of initial stage treatment, which we decided to perform surgery (laparoscopic Strong’s operation). The postoperative period was without complications. The patient noted an improvement in the state and the relief of pain in the epigastrium and was discharged after 9 days of hospitalization in satisfactory condition.
Conclusion. For diagnosis and treatment in time as well as prevention of possible complications, it is necessary to improve surgeons’ information about this pathology, which if diagnosed and treated late can lead to severe, life-threatening complications up to death. The diagnosis at the initial stages, specifically with the assistance of computer tomography with contrast, angiography, and treatment in a timely manner, can preserve life and prevent the possible outcomes of fatal complications.
Keywords
For citations:
Galimov O.V., Khanov V.O., Karkhani H.H., Bhawna Sh., Ibragimov T.R. The Complication Of Decrease In Aorto-Mesenteric Angle And Distance Its Diagnosis And Treatment: Case Report. Creative surgery and oncology. 2022;12(2):123-127. https://doi.org/10.24060/2076-3093-2022-12-2-123-127
INTRODUCTION
The superior mesenteric artery syndrome (SMAS), Wilkie’s syndrome (WS) is a rare pathological condition that involves the horizontal part of duodenum which is compressed between the superior mesenteric artery (SMA) and abdominal aorta, there can be spine involves in the compression in some cases; which leads to the hindrance for the passage of himus in the duodenum, creating a mechanical obstruction, causes widening and destruction of intestine and stomach [1–3]. The SMA supplies the horizontal part of the duodenum, pancreas, and two-third of the transverse colon. The causes of developing SMAS are mostly rapid and excessive weight loss, resulting in the loss of the duodenal fat pad [4–7]. The reduction of the fat pad cells therefore leads to the changes in angle between the abdominal aorta and the SMA, or aorto-mesenteric angle and distance, causing intestinal obstruction. The Classic symptoms of acute SMAS include postprandial abdominal pain, nausea, and vomiting. It can be congenital or acquired [8][9].
The literature data on the frequency of occurrence of the WS is widely different and is estimated at 0.1 % to 0.78 % in various studies [10][11]. Various authors write that it is detected in 3–17 % of cases among the causes of chronic ileus and in 0.013–0.30 % of cases with radiological studies of the upper gastrointestinal tract (GIT) [6][12][13]. The combination of chronic ileus with stomach ulcer disease is observed in 25–75 %, with a duodenal ulcer in 31–39 %, with a biliary disease of 8.9–87.4 %, and hyperchlorhydria up to 50 % [8][11][14]. The ratio of women suffering from WS is two times greater than that of men. In up to 75 % of cases, the disease is detected in the age group of 10 to 30 years. However, this syndrome can be seen in 84-year-old and 86-year-old patients. This pathology is not only a rare disease, but also a frequently unfamiliar situation for many surgeons because the patients can develop life-threatening complications that can lead them to death by up to 33 % [8][15][16].
MATERIALS AND METHODS
Patient G, a 28-year-old man, was admitted to the surgical department of the Bashkir State Medical University (BSMU) clinic on October 11, 2021, with complaints of postprandial abdominal pain in the epigastric region, which was radiating to the lower back, belching, bloating, and nausea. He complained of difficulty breathing and periodic pain behind the sternum associated with meals. The patient also notes progressive weight loss. He suffered from Osteochondrosis, left-sided scoliosis, an acute coronavirus infection in September 2021. No history of smoking or alcohol, and had no allergic reaction. The symptoms first appeared in 2018 and worsened day by day.
The results of the inspection during admission: Height 173 cm, weight 60 kg, Body Mass Index (BMI) 20 kg/m2; the body temperature was 36.7°C. Heart rate was 74 beats per minute. Blood pressure: 120/75 mm Hg. The abdomen was soft during palpation and moderately painful in the epigastric region; no symptoms of peritoneal irritation were seen. During auscultation of bowel sounds, the intestinal peristalsis was heard. The kidney punch test was negative. Diuresis was normal.
Diagnosis
Esophagogastroduodenoscopy in dynamics shows hypertrophic and superficial gastritis, gastroduodenal reflux. Therapy was carried out with proton pump inhibitors, after 2 weeks, the signs of aggravation of gastritis went, but the pain persisted. The ultrasound shows increased pneumatization in the intestine. X-ray shows R-signs of gastritis. Echocardiography and Electrocardiography were normal. MRI of the thoracic vertebra: signs of initial manifestations of degenerative changes in the thoracic spine. Left-side spondylarthrosis Th4–Th9. The abdominal CT-scan with combined contrast of the stomach and duodenum per os with water-soluble contrast and computer angiography of the mesenteric vessels shows decrease in the aorta-mesenteric angle to 14° (normal 35–65°) (Figure 1); the distance between these vessels at the origin was 6 mm (normal 10–28 mm) (Figure 2a, b). There was a compression of the left renal vein between these vessels: the diameter at the compression level was 0.2–0.3 cm, and the diameter of the veins present more proximally to the origin of the SMA was 1.2 cm moderate compression of the lower horizontal part of the duodenum.
These findings show the patient was suffering from Superior mesenteric artery syndrome (Wilkie syndrome) with moderate compression of the duodenum and the left renal vein (Nutcracker syndrome).
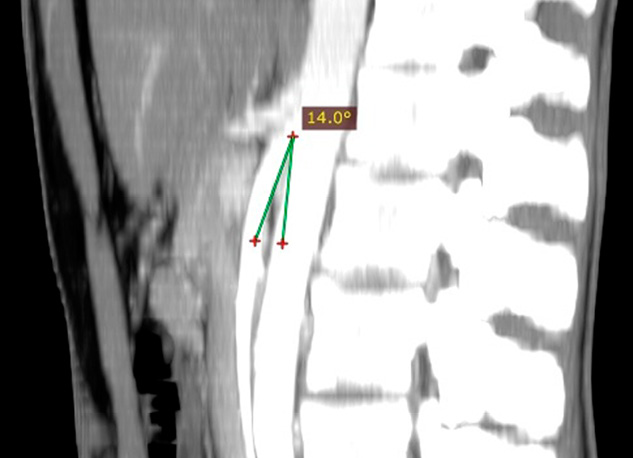
Figure 1. Sagittal section of CT-scan with contrast of the abdomen (peritoneum and retroperitoneal space) showing a narrowed Aorto-mesenteric angle of 14°
Рисунок 1. Контрастная КТ брюшной полости (брюшина и забрюшинное пространство), сагиттальная проекция; суженный аорто-мезентериальный угол 14°
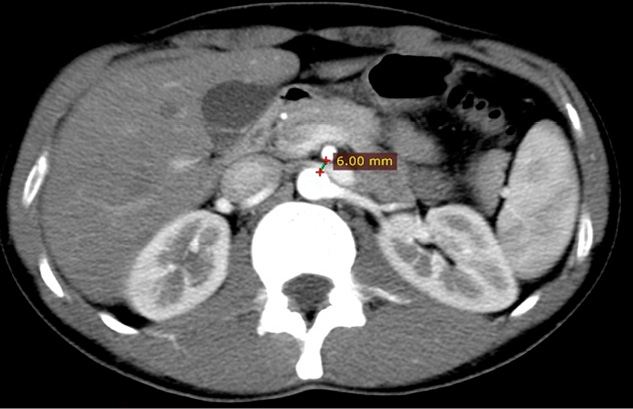
Figure 2a. Axial section of CT-scan with contrast of the abdomen (peritoneum and retroperitoneal space) showing a narrowed Aorto-mesenteric distance of 6.0 mm
Рисунок 2а. Контрастная КТ брюшной полости (брюшина и забрюшинное пространство), аксиальная проекция; суженное аорто-мезентериальное расстояние 6,0 мм

Figure 2b. Sagittal section of CT-scan with contrast of the abdomen (peritoneum and retroperitoneal space) showing a narrowed Aorto-mesenteric distance of 6.0 mm
Рисунок 2b. Контрастная КТ брюшной полости (брюшина и забрюшинное пространство), сагиттальная проекция; суженное аорто-мезентериальное расстояние 6,0 мм
Course of operation
Laparoscopic Strong operation was performed as it has minimal invasion and with less complications as compared to others, the anastomosis done by laparotomy. As a preoperative preparation, the patient had been given antibiotics for the prevention of thromboembolic complications; the compression linen was applied 30 minutes before the operation. A planned operation was carried out under endotracheal anesthesia. Laparocentesis was performed with a paraumbilical trocar of 10 mm CO2 insufflation was done at 10–12 mm Hg. Under visual control, a laparoscope was introduced, as well as two 5 mm and one 10 mm trocars. During the inspection, there was compression of the duodenum by the SMA. The horizontal part of the duodenum was expanded to 5–6 cm below the ligament of Treitz; the diameter of the small intestine was around 2 cm. The procedure of the Strong operation was performed by mobilizing the horizontal part, by dividing the ligament of Treitz, preparing for the imposition of an anastomosis. A mini laparotomy was performed over an anastomosis overlay area, after which the Duodenojejunostomy was done and the compressed portion of the duodenum was released. Hemostasis was controlled. A tubular drain was installed in the abdominal cavity; the abdominal wall was stitched layer by layer, and aseptic dressings were applied. The postoperative period was without complications. Symptomatic drug therapy was carried out; everyday dressing of the postoperative wound with antiseptics was performed. Postoperative ultrasound was done to check free fluid and to know if the symptoms were relieved or not, the intestinal loops were expanded or not; the patient noted an improvement in the state and the relief of pain in the epigastrium; there were no complaints about nausea and vomiting. He was discharged after 9 days of hospitalization in satisfactory condition, and advised to have an X-ray of the abdomen after a month, as follow up routine checkup to see if the symptoms would reoccur. During the inspection, there were no complaints of pain or discomfort, and no clinical signs were seen that were present before the operation. Weight gain was noted up to 61 kg, no anorexia, no signs of postprandial pain, or epigastric tenderness.
RESULTS AND DISCUSSION
WS is commonly known in the literature as chronic duodenal intestinal obstruction, CAST syndrome, superior mesenteric artery syndrome, duodenal vascular compression, duodenal aorto-mesenteric compression, and chronic duodenal vascular compression. WS is manifested by compression of the transverse part of the duodenum when it passes through the area between the abdominal aorta, spine, and SMA [1][8][10]. Due to the decrease in aorto-mesenteric angle and distance, the normal angle of SMA branch out from the aorta ranges usually from 38 to 80 degrees. The aorto-mesenteric distance varies from 10 to 28 mm, but when the angle of the SMA branch out from the aorta is less than 22 degrees and the distance is less than 8 mm, it creates conditions of chyme passage hindrance along the duodenum, thus creating mechanical obstruction of the duodenum [5][8][14]. Absence of timely diagnosis of this disease can lead to life-threatening complications, and early diagnostics is complicated by the similarity of initial manifestations with other gastropancreaticoduodenal diseases. One of the most promising approaches in the diagnosis of WS is the use of abdominal CT with combined contrast of the stomach and duodenum per os with water-soluble contrast and computer angiography of the mesenteric vessels. In the present clinical case, due to the given combination of methods, we can assess the functional state of the stomach and duodenum, clearly visualize not only the organ topography but also estimate the aorto-mesenteric angle and distance, which can further determine the type and tactics of initial stage treatment, in which we decided to perform surgery (laparoscopic Strong’s operation). The postoperative period proceeded without any complications. The patient noted improvement in his condition and the absence of pain in the epigastrium and was discharged 9 days after hospitalization in satisfactory condition.
CONCLUSION
This pathology is not only a rare disease, but also a frequently unfamiliar situation for many surgeons because patients can develop life-threatening complications that can lead them to death by up to 33 % [1][3][6]. The decrease in distance and the aorto-mesenteric angle can develop not only duodenal hypertension but also renal vein compression, which leads to renal fornical hemorrhage and varicocele, which can lead to reproductive pathologies [4][6][8]. It can be hard to diagnose at once, but with proper clinical investigations, the diagnosis can be made as in the case above. With the treatment of Strong’s surgery; there was reduction in symptoms and pain, and the patient gained weight and increase in BMI by diet change. Thus, timely treatment can save the time and life of the patient.
Statement of informed consent. Written informed consent was obtained from the patient for publication of this case report and accompanying materials.
Conflict of Interest. The authors declare no conflict of interest.
Sponsorship Data. This work is not funded.
References
1. Karki B., Pun B., Shrestha A., Shrestha P.S. Superior mesenteric artery syndrome. Clin Case Rep. 2020;8:2295–7. DOI: 10.1002/ccr3.3118
2. Farina R., Iannace F.A., Foti P.V., Conti A., Inì C., Libra F., et al. A case of nutcracker syndrome combined with wilkie syndrome with unusual clinical presentation. Am J Case Rep. 2020;21:e922715. DOI: 10.12659/AJCR.922715
3. Ryabykh S.O., Scryabin E.G., Chevzhik V.P., Filatov E.Y. Arteriomesenteric compression of the duodenum as a complication of the surgical correction of typical idiopathic scoliosis: clinical case. Hirurgia Pozvonochnika. 2020;17(2):6–14 (In Russ.). DOI: 10.14531/ss2020.2.6-14
4. Hamidi H., Tareq Rahimi M., Maroof S., Ahrar Soroush F. Computed tomography features and surgical treatment of superior mesenteric artery syndrome: A case report. Radiol Case Rep. 2019;14(12):1529–32. DOI: 10.1016/j.radcr.2019.09.036
5. Bhatt S., Mishra B., Tandon A., Manchanda S., Parthsarathy G. Superior mesenteric artery syndrome in association with abdominal tuberculosis: an eye opener. Malays J Med Sci. 2017;24(3):96–100. DOI: 10.21315/mjms2017.24.3.12
6. Habib A.E., Din M.N. Superior mesenteric artery syndrome caused by acute weight loss in a 16-year-old polytrauma patient: A rare case report and review of the literature. Ann Med Surg. 2021;65:102284. DOI: 10.1016/j.amsu.2021.102284
7. Hangge P.T., Gupta N., Khurana A., Quencer K.B., Albadawi H., Alzubaidi S.J., et al. Degree of left renal vein compression predicts Nutcracker syndrome. J Clin Med. 2018;7(5):107. DOI: 10.3390/jcm7050107
8. Warncke E.S., Gursahaney D.L., Mascolo M., Dee E. Superior mesenteric artery syndrome: a radiographic review. Abdom Radiol (NY). 2019;44(9):3188–94. DOI: 10.1007/s00261-019-02066-4
9. Bhagirath Desai A., Sandeep Shah D., Jagat Bhatt C., Umesh Vaishnav K., Salvi B. Measurement of the distance and angle between the aorta and superior mesenteric artery on CT scan: values in indian population in different BMI categories. Indian J Surg. 2015;77(Suppl 2):614–7. DOI: 10.1007/s12262-013-0941-1
10. Esmat H.A., Najah D.M. Superior mesenteric artery syndrome caused by acute weight loss in a 16-year-old polytrauma patient: A rare case report and review of the literature. Ann Med Surg (Lond). 2021;65(102284):102284. DOI: 10.1016/j.amsu.2021.102284
11. Mohtashami A., Chui J.N., Law C., Cole-Clark D., Simon R. Postoperative superior mesenteric artery syndrome following appendicectomy: A case report. Int J Surg Case Rep. 2022;90(106629):106629. DOI: 10.1016/j.ijscr.2021.106629
12. Yan C., Hu Z.-W., Wu J.-M., Zhang C., Yan L., Wang Z.-G. Laparoscopic Toupet fundoplication with duodenojejunostomy for the management of superior mesenteric artery syndrome with reflux symptoms. Medicine (Baltimore). 2017;96(3):e5771. DOI: 10.1097/MD.0000000000005771
13. Hidayatullah H., Mohammad T.R., Sahar M., Freba A.S. Computed tomography features and surgical treatment of superior mesenteric artery syndrome: A case report. Radiology Case Reports.2019;14:1529–32. DOI: 10.1016/j.radcr.2019.09.036
14. Xu M.M., Dawod E., Gaidhane M., Tyberg A., Kahaleh M. Reverse endoscopic ultrasound-guided gastrojejunostomy for the treatment of superior mesenteric artery syndrome: a new concept. Clin Endosc. 2020;53(1):94–6. DOI: 10.5946/ce.2018.196
15. Cicero G., D’Angelo T., Bottari A., Costantino G., Visalli C., Racchiusa S., et al. Superior mesenteric artery syndrome in patients with Crohn’s disease: a description of 2 cases studied with a novel magnetic resonance enterography (MRE) procedure. Am J Case Rep. 2018;19:431–7. DOI: 10.12659/ajcr.908273
16. Druckera N.A., Marine M.B., Rescorla F.J. Gastric pneumatosis: An unusual presentation of superior mesenteric artery syndrome. J Pediatr Surg Case Reports. 2018;36:25–7. DOI: 10.1016/j.epsc.2018.06.014
About the Authors
O. V. GalimovRussian Federation
Dr. Sci. (Med.), Prof., Department of Surgical Diseases and New Technologies with a course of Advanced Professional Education
Ufa
V. O. Khanov
Russian Federation
Dr. Sci. (Med.), Prof., Department of Surgical Diseases and New Technologies with a course of Advanced Professional Education
Ufa
H.M. H. Karkhani
Russian Federation
Department of Surgical Diseases and New Technologies with a course of Advanced Professional Education
Ufa
Sh. Bhawna
Russian Federation
Graduate Student (6th year)
Ufa
T. R. Ibragimov
Russian Federation
Department of Surgical Diseases and New Technologies with a course of Advanced Professional Education
Ufa
Review
For citations:
Galimov O.V., Khanov V.O., Karkhani H.H., Bhawna Sh., Ibragimov T.R. The Complication Of Decrease In Aorto-Mesenteric Angle And Distance Its Diagnosis And Treatment: Case Report. Creative surgery and oncology. 2022;12(2):123-127. https://doi.org/10.24060/2076-3093-2022-12-2-123-127
JATS XML


































